Disease
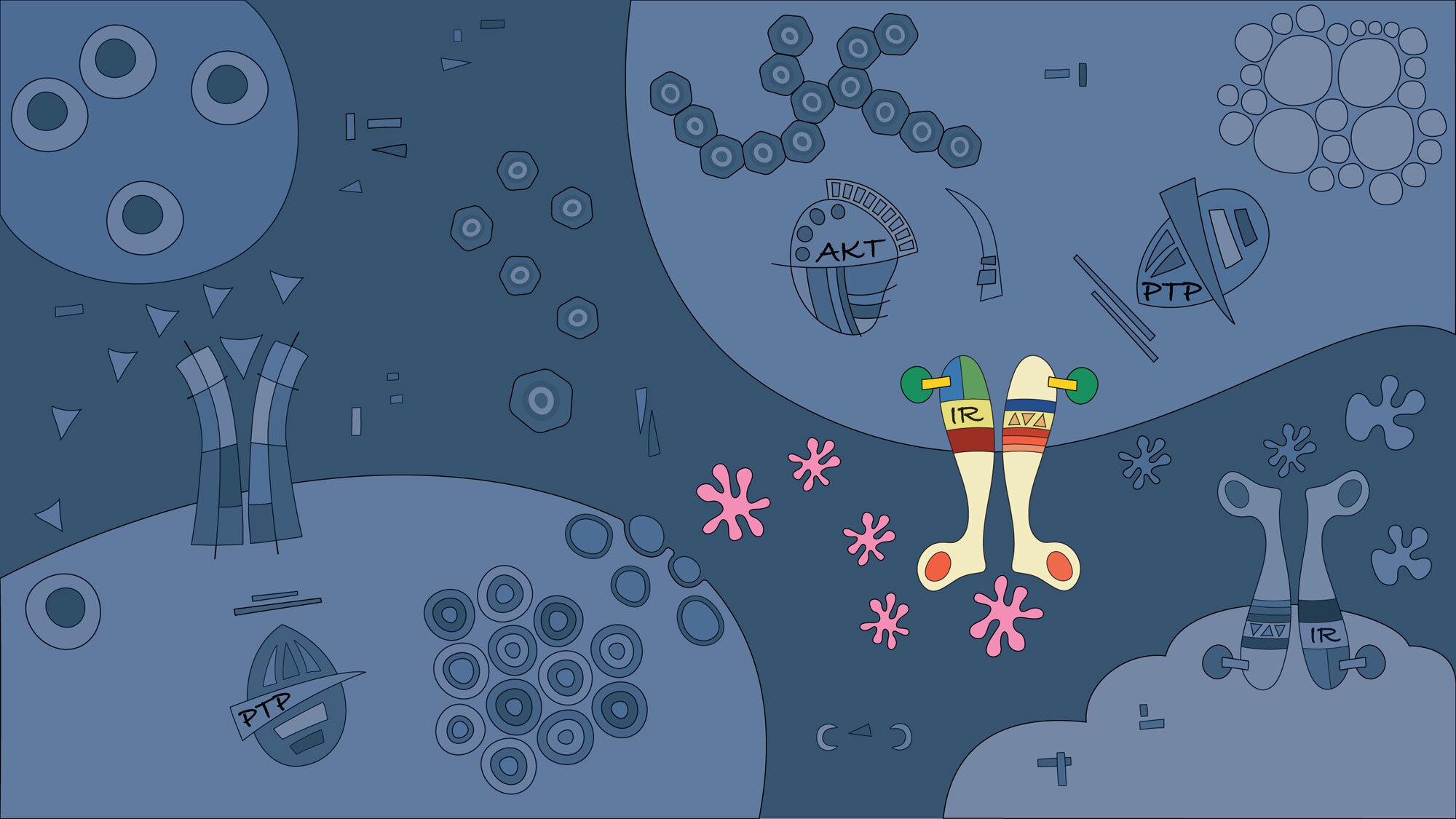
Great efforts have been made to understand how different cell types control signalling pathways in the context of metabolic disorders such as obesity, diabetes, and liver cancer, but the molecular mechanisms by which these pathologies occur remain poorly understood.
We face the challenge of very heterogeneous diseases that require a deep understanding of the pathologies to find creative diagnostic and therapeutic strategies.
“Cures for disease flow out of progress in understanding as the natural fruits of knowledge”
Type 1 Diabetes
Type 1 diabetes accounts for 10-15% of cases and results from progressive autoimmune destruction of insulin-producing β cells in the islets of Langerhans of the pancreas. Without β-cell function, patients with type 1 diabetes are dependent on insulin injections to control their blood sugar levels.
Researchers at the Signal Transduction and Metabolism Laboratory are dedicated to finding effective detection, prevention and treatment strategies for type 1 diabetes. Research at the laboratory incorporates basic and clinical studies, using both rodent and human cells to study the causes and mechanisms of the disease and to explore new treatment and diagnostic options. Learn more about our research.
Type 2 Diabetes
High blood glucose in type 2 diabetes results from resistance to the effects of insulin in the liver, muscle, and adipose tissue in combination with failure of the β cells to produce enough insulin. Approximately 80% of diabetic patients have type 2 diabetes, with sixty million Europeans suffering from the disorder.
Type 2 diabetes has a genetic predisposition, but the risk is greatly increased with excess weight or obesity, insufficient physical activity, unhealthy diet and age. The increasing prevalence of obesity in society means that the incidence of type 2 diabetes is expected to increase further, as are the associated public health burden and economic costs. The development of type 2 diabetes is complex and involves an interplay between multiple signalling pathways and tissues. There is no cure for this disease. Therefore, intensive scientific research and new treatments need to be developed for these patients. Learn more about our research.
Hepatocellular carcinoma
Hepatocellular carcinoma (HCC) accounts for 90% of primary liver cancers and is refractory to nearly all currently available anticancer therapies with a 5-year survival rate of nearly 15%. Over the last 20 years, the incidence of HCC has been rapidly increasing in economically developed nations and is mostly attributable to hepatitis C virus (HCV), alcoholic, and metabolic dysfunction-associated steatotic liver disease (MASLD). With the development of novel antiviral therapies against HCV, the obesity epidemic is thought to now account for as much as 40% of the increase in HCC in developed countries.
A hallmark of MASLD is the accumulation of fat in hepatocytes (liver cells). Indeed, the main risk factors for MASLD are obesity and type 2 diabetes, which can progress to fibrosis, metabolic dysfunction-associated steatohepatitis (MASH), cirrhosis, and HCC. The mechanisms that underpin the progression from obesity to MASH and HCC in obesity/type 2 diabetes involve genetic and environmental factors that influence disease severity and progression. Learn more about our research.
Support our research
You have the opportunity to become a supporter of the work being undertaken at the Signal Transduction & Metabolism Laboratory - your support will help the new generation of junior researchers become experienced scientists and may make a difference in the search of better treatments for diabetes and liver cancer.




